How is the diagnosis of glaucoma established and how is the disease monitored ?
The ophthalmologist establishes the diagnosis of glaucoma based on a number of specific examinations to assess the status of the optic nerve and the presence of risk factors (intra-ocular pressure). By repeating the same examinations over time and comparing the results with the initial outcomes, the ophthalmologist is able to judge whether the disease is stable or progressive.
Measurement of intra-ocular pressure
The intra-ocular pressure is measured with a tonometer, a device that gently presses against the convex cornea in order to obtain a certain amount of flattening; the intra-ocular pressure is derived from the force required to obtain the corneal flattening. Before making contact with the eye a drop of anaesthetic solution is instilled so that the procedure is completely painless. As a patient you only see a blue light approaching but you do not feel anything. Naargelang het oog zich gemakkelijk of moeilijk laat indrukken, zal de oogarts een lagere of een hogere waarde voor de oogdruk aflezen op de schaal van de tonometer.
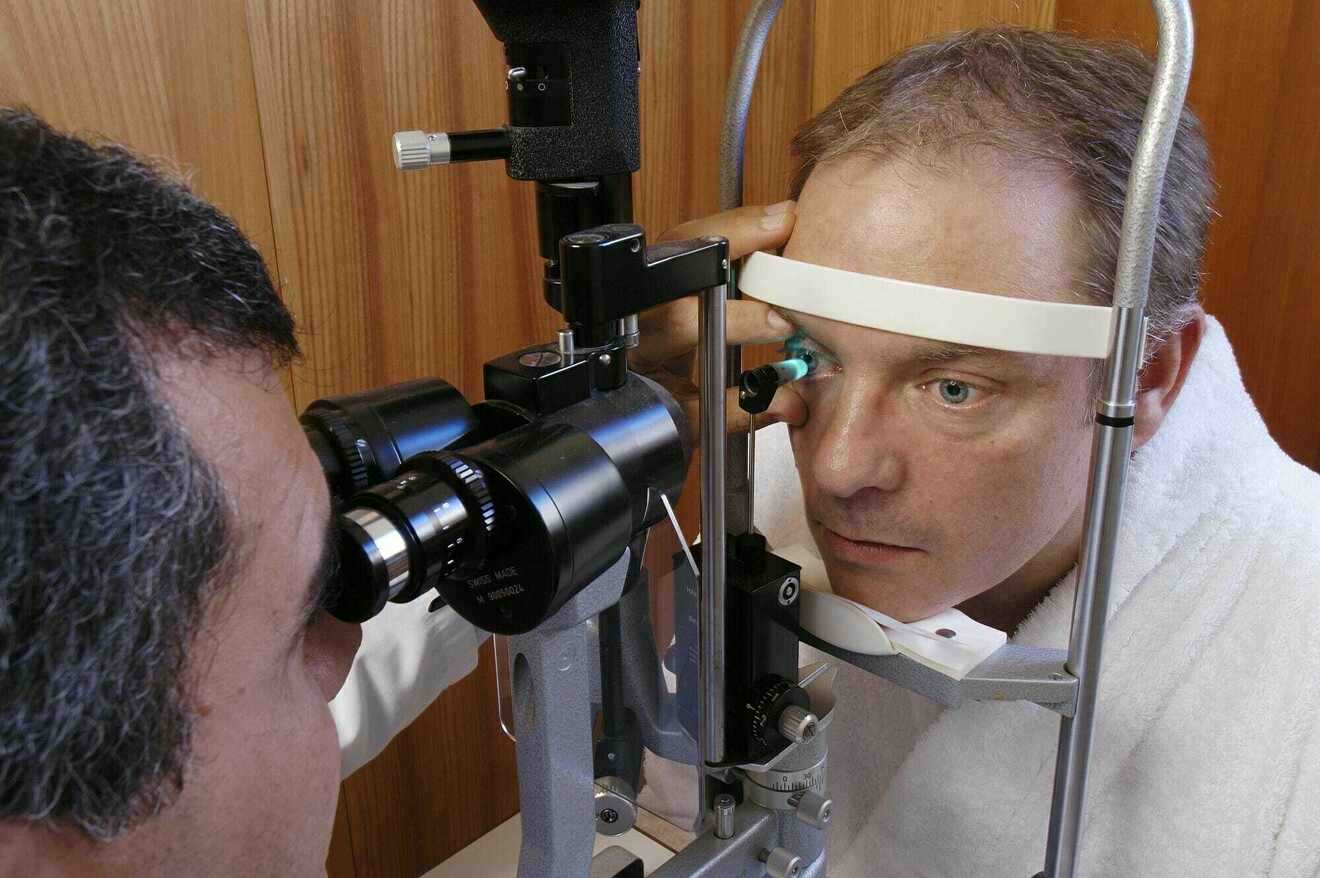
Another method to measure the intra-ocular pressure is by exposing the cornea to a sudden puff of air to obtain flattening of the cornea. Since there is no contact with the eye there is no need for anaesthetic drops. This method, called pneumotonometry, is less accurate than the classic method described above.
Evaluation of optic nerve damage
With the appropriate instruments and lenses the ophthalmologist is able to visualize the inner eye and to observe the retina and the optic nerve head (= optic disc). Glaucomatous damage of the optic nerve causes a hollowing and widening of the normal central dimple of the optic disc, a process called optic disc excavation. Excavation is a diagnostic sign of glaucoma and progressive excavation upon subsequent examinations indicates an ongoing loss of optic nerve fibres which means that the disease is not under control with the current treatment. Therefore, examination of the optic disc appearance is a key element in the diagnosis and the follow up of glaucoma. In order to facilitate objective comparisons of the optic disc over time the ophthalmologist may take a photograph. Dilation with eye drops is sometimes required to ensure good visibility of the inner eye. This procedure is painless but you may experience blurry vision in the first hours. Therefore it is prudent not to drive home yourself after dilation of the pupil.



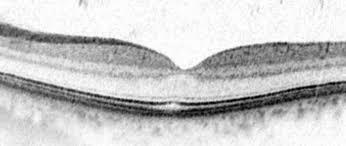
Evaluation of the nerve fibre layer
Modern imaging techniques allow us to visualize the different layers of the retina with Optical Coherence Tomography or OCT. The OCT machine enables us to measure the thickness of the nerve fibre layer, to detect early loss of nerve fibres, and to monitor whether the loss is stable or ongoing. Comparison of the thickness of the nerve fibre layer over time indicates whether the disease is sable or not under the current treatment. OCT technology is based on coherent light rays and hence is completely harmless.

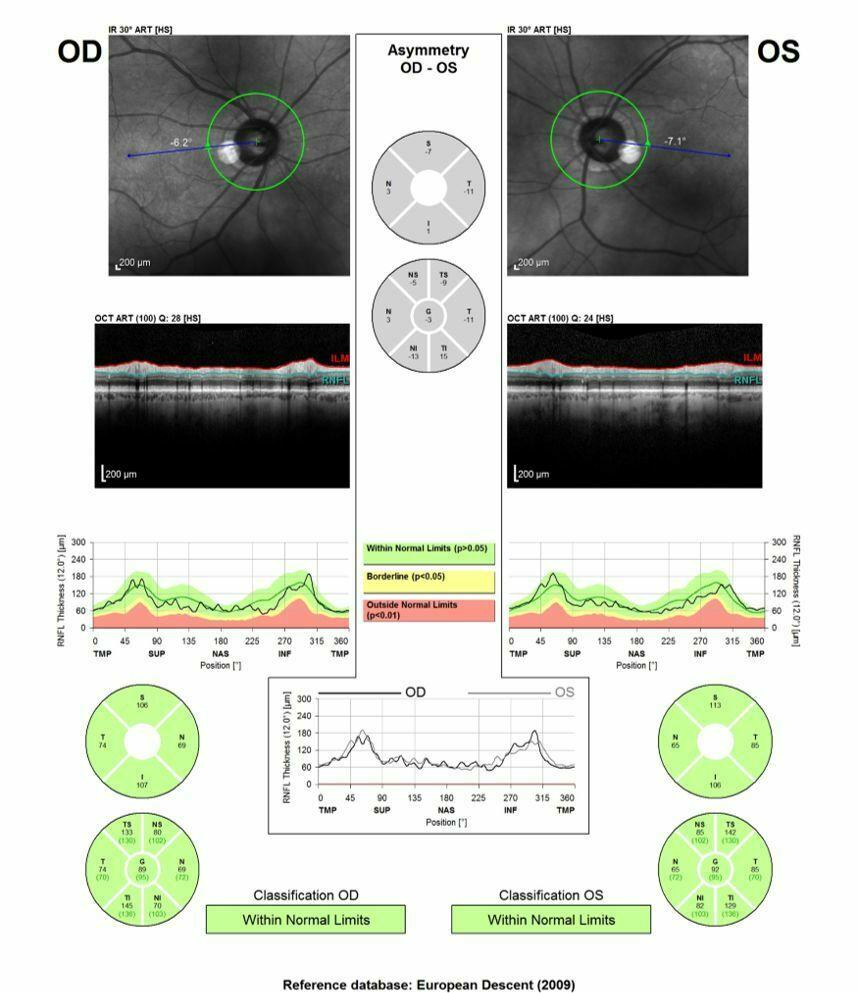
Outprint of the OCT of a normal subject (OD = right eye, OS = left eye). Above is a picture of the retina with a green circle around the disc which visualizes the scanning track; the retinal layers are displayed in the middle of the outprint; the bottom part shows a pie-chart that represents the nerve fiber layer thickness in the different quadrants; the green colour stands for normal thickness of the nerve fiber layer.
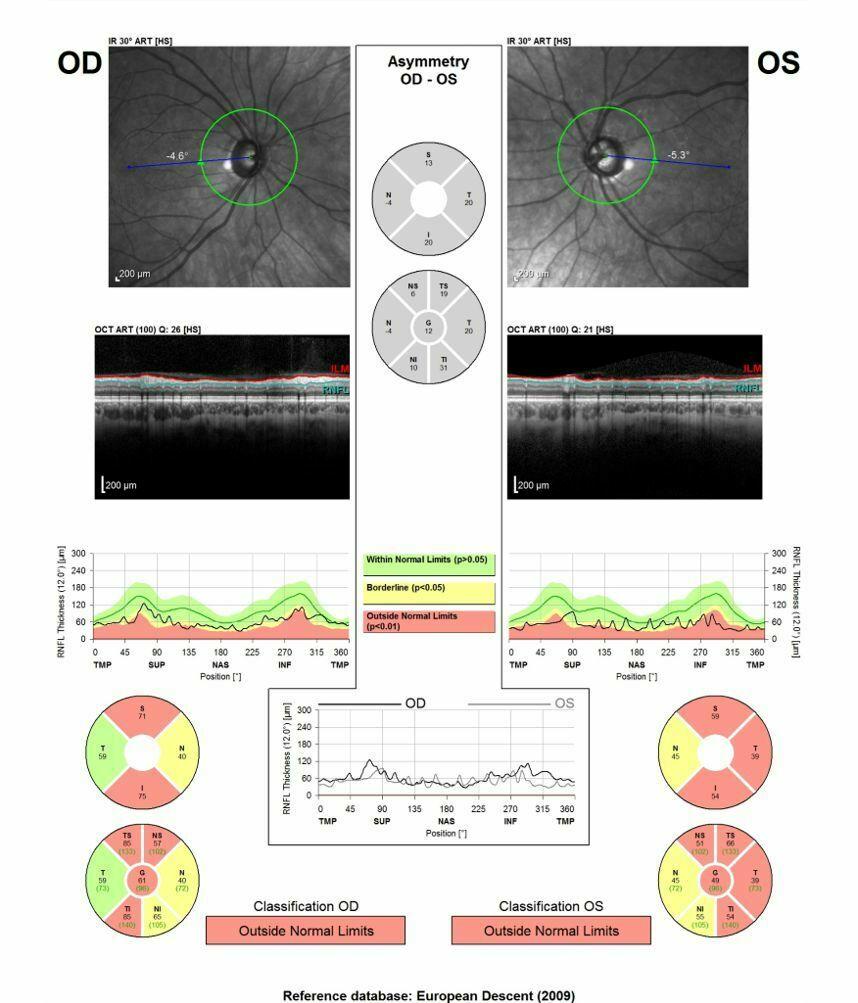
OCT outprint of a patient with glaucoma; the pictures of the retina clearly show excavation of the disc left eye more than right; the red sectors indicate areas of profound nerve fiber loss; the yellow sectors are borderline and hence suspect. Note that the greater excavation of the left eye goes hand in hand with a more pronounced nerve fiber loss on OCT (more red)
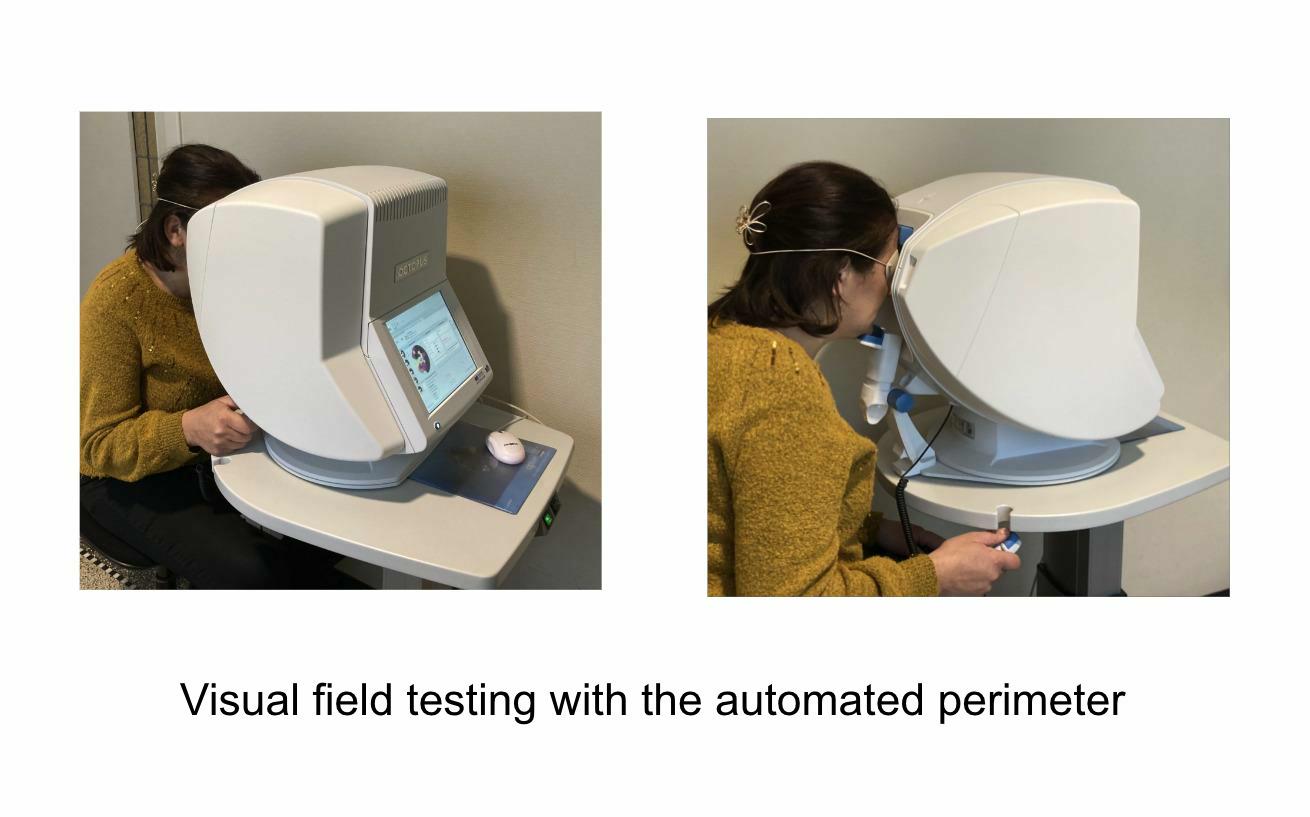
Evaluation of the loss of sight
Evaluation of the visual field (= perimetry) with the automated perimeter is able to detect areas of decreased sensitivity to light very early, long before you become aware of it. The perimeter is a hemisphere against which small light stimuli of variable size and intensity are projected one by one. Your head is stabilized in a chin rest and one eye is occluded. The other eye fixates a central point of the hemisphere. Each time you see a light you have to press a button, always maintaining central fixation. This examination which may take up to ten minutes per eye, is rather stressful and requires a fair amount of cooperation from your side. Visual field data however are extremely relevant to document whether glaucomatous damage is present or not, and if present, how severe it is. The data of each examination are stored in the computer for statistical analysis and comparison of visual fields over time will allow your ophthalmologist to conclude whether or not the disease is under control with the treatment applied.


Evaluation of the anterior chamber angle
The ophthalmologist puts a special lens on your eye after instillation of anaesthetic drops to visualize the drainage structures located in the angle between the iris root and the cornea over the entire 360°. This examination is particularly important to distinguish different types of glaucoma, especially to make the distinction between open-angle glaucoma (drainage structures clearly visible between iris root and cornea) and angle-closure glaucoma (drainage structures hidden from view by adhesions between iris root and cornea). See also below, acute angle-closure glaucoma.
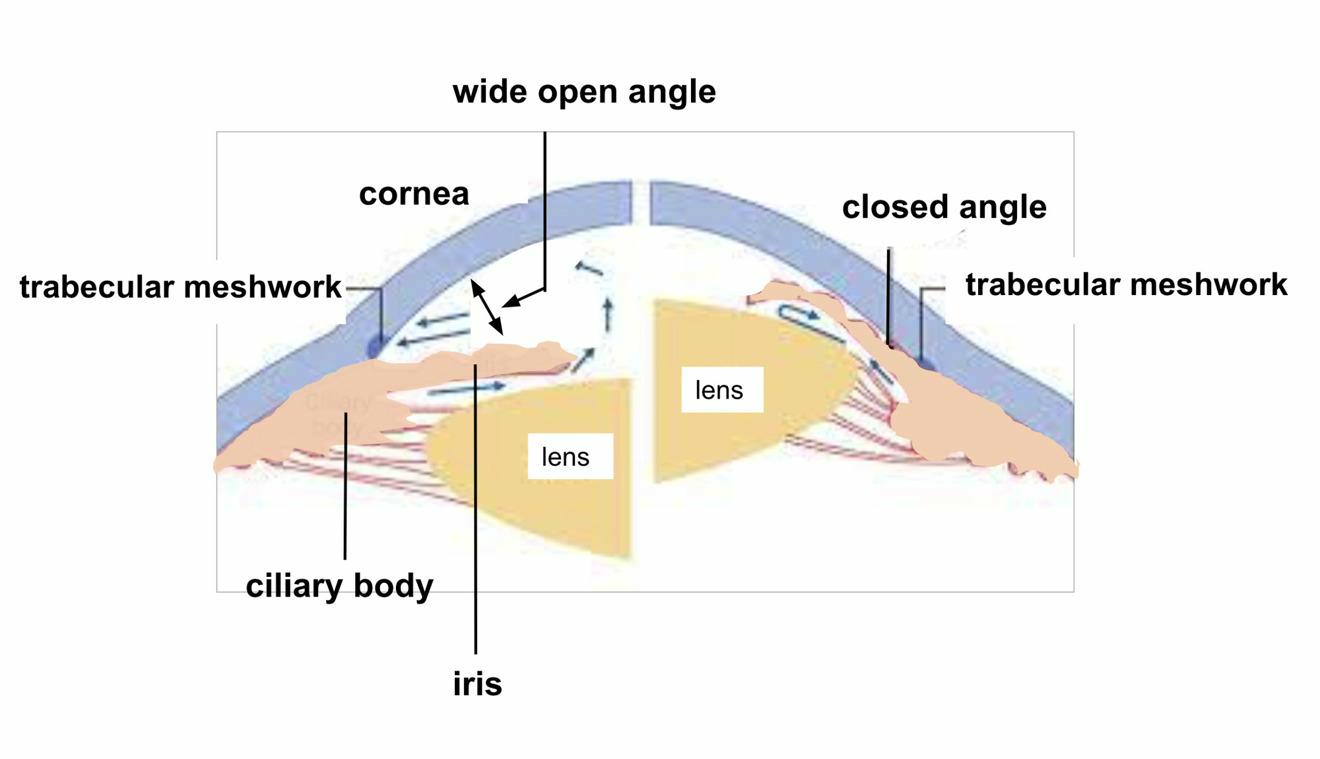
The drawing on the left shows a normal anterior chamber with a wide open angle; the drawing on the right shows a very narrow angle with adhesions between the base of the iris and the peripheral cornea. (also see acute angle-closure glaucoma)
Measurement of corneal thickness
The thickness of the cornea has an impact on the intra-ocular pressure readings: if your cornea is thicker than normal the pressure readings will be higher than your actual intra-ocular pressure. Vice versa, if your cornea is thinner than normal the tonometer readings will underestimate the real pressure. Corneal thickness is measured with an ultrasound or an optical device. Both methods are quick and painless. Since corneal thickness does not change much over time it needs to be measured only once.
How often are these examinations repeated during follow up of my glaucoma?
Depending on the severity of the disease tests are repeated one to four times a year to determine if the current treatment is effective in halting further damage to the optic nerve. If not, treatment modalities will be adapted until the disease is under control, which means no further deterioration of the visual field, no increase in optic disc excavation and no further nerve fibre loss on OCT. Once this stable situation under treatment is reached it is recommended to have a check of the optic disc and the intra-ocular pressure twice a year. Visual field examination should be repeated every year, ideally completed with imaging of the nerve fibre layer.
